Suśruta on Determining Envenomation Status of a Patient
The most common argument doctors, herpetologists, and global health authorities use against traditional medicine is that it only seems to work because most of the time the snake doesn’t inject a lethal amount of venom. The implication, of course, is that traditional doctors are completely ignorant of this fact, or know it and don’t let on in order to trick their patients with false success stories. Unfortunately this initially persuasive argument has little basis in reality and can easily be turned around by saying that antivenom only seems to work because most of the time a lethal amount of venom is not injected. I am well aware that in an ideal world the doctor will only use antivenom when signs of envenomation are present, when the snake species is identified as one treatable by the available antivenom, and when it has been determined that the patient will not have an acute allergic response to the antivenom. Unfortunately we don’t live in such an ideal world. A recent report on snakebite in Cambodia (linked) revealed the shocking news that NONE of the antivenom available and IN USE in Cambodia as of 2009 is valid for Cambodian snakes. The article also featured a chart on the outcomes of snakebite cases in the few hospitals in Cambodia keeping records of it, and usually the death rate was fairly low (<10%) to medium (20%). Since they were using the wrong antivenom in many cases, and the doctors were often unsure about how to use the antivenom, how many of the deaths might be attributed to allergic reaction to the “medicine”? Not an ideal world at all.
My point here is NOT to argue that one shouldn’t go to the hospital for antivenom treatment, but at the same time we cannot accept invalid arguments from a medical industry in which things like the Cambodia example can happen. Dismissing traditional medicine out of hand, which is to say without having any knowledge of it, is unscientific. Scrupulous scientists will agree and desire to test the various medicines used in a given traditional pharmacology. See my preliminary list of some such evaluations here.
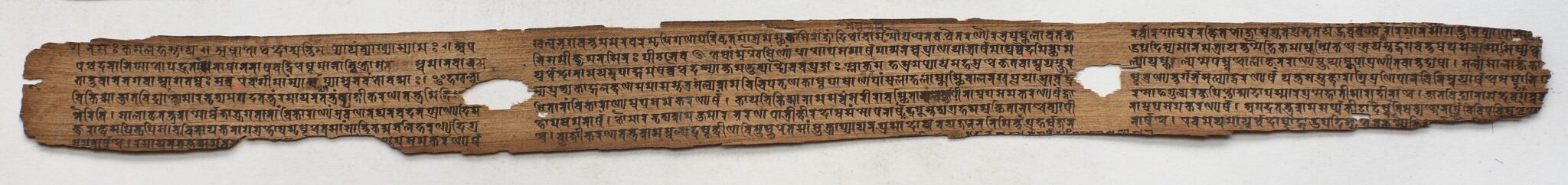
For my part, let me start by pointing out a striking passage in the Suśrutasaṃhitā, dating back at least 1,800 years and still in use among physicians of Āyurveda. This passage nicely illustrates the awareness of determining envenomation status in a spiderbite victim:
lūtāviṣaṃ ghoratamaṃ durvijñeyatamaṃ ca tat |
duścikitsyatamaṃ cāpi bhiṣagbhirmandabuddhibhiḥ ||5.8.75
saviṣaṃ nirviṣaṃ caitadityevaṃ pariśaṅkite |
viṣaghnameva kartavyamavirodhi yadauṣadham || 5.8.76
agadānāṃ hi saṃyogo viṣajuṣṭasya yujyate |
nirviṣe mānave yukto ‘gadaḥ saṃpadyate ‘sukham || 5.8.77
tasmāt sarvaprayatnena jñātavyo viṣaniścayaḥ |
ajñātvā viṣasadbhāvaṃ bhiṣagvyāpādayennaram || 5.8.78
“Spider venom is extremely vehement and difficult to diagnosis, and it is nearly impossible for dim-witted doctors to cure it. Thinking ‘Is the patient envenomed or not?’ he wavers on which poison-destroying medicine could be used without causing problems. Indeed, the use of antidotes is indicated for one who is envenomed, [but] an antidote used on a person that is not envenomed will cause trouble. Therefore all efforts should be used to settle the diagnosis of envenomation. If the doctor does not know the true state of envenomation, he might kill the man.”
Tags